Geostatistical Exploratory Analysis on Child Malnutrition and its Determinants in India
Mandadi, R. R., 1* Tripathi, N. K., 2 Pal,
I., 3 Mozumder, C. 4 and Gonzales, A. L.5
Asian Institute of Technology, Thailand
* Corresponding Author
Abstract
Child malnutrition is often the most common factor that causes
child mortality rate. In the study of child malnutrition, there is
limited evidence on spatial analysis to identify spatial trends and
hotspots of indicators and contextual factors contributing to
geographical inequalities in child malnutrition.
This study aims to investigate the spatial distribution and
heterogeneity of Malnutrition across districts and states of India
and examine the influence of determinants on wasting, stunting, and
underweight children under five-year-of age. The spatial variation
in Malnutrition and the influencing determinants were determined
across India at district levels using the National Family Health
Survey 3 and 4 (2006–16) data. Results show that out of the 640
districts in India, a very high prevalence of stunting, wasting,
and underweight occurs in 236, 472, and 370 districts,
respectively. The spatial error regression model showed that
maternal health, such as low mother BMI, anemia during pregnancy,
absence of antenatal care, early marriage and pregnancy, and lack
of improved sanitation facilities in the household, were the most
significant factors influencing Malnutrition in India. Furthermore,
the Bivariate LISA analysis revealed that malnutrition prevalence
was higher in the geographical pockets where maternal care is low
and mainly clustered in the country's western, central, and eastern
districts. The influencing factors in every malnutrition indicator
vary in different districts. A notable observation was that the
factors influencing a larger spatial scale (state level) might not
necessarily be the attributing factors to the prevalence and
occurrence of Malnutrition at a smaller spatial scale (district
level). The geocoded data is more detailed using household level was
used to show the chronic areas of Malnutrition and develop a
strategy/policy to reduce Malnutrition efficiently.
Keywords: Child Malnutrition, Choropleth Map, Spatial
Analysis, Stunting Underweight and Wasting
1. Introduction
Malnutrition is one of the most critical conditions and is responsible
for higher mortality levels; children under five years are vulnerable
to Malnutrition. Malnutrition is the primary cause of a child's death
as it lowers infection resistance and is a socio-economic problem
restricting development worldwide [1]. Child malnutrition manifests as
being underweight, stunting, and wasting, a clinical sign of nutrient
deficiency [2]. The World Health Organization [3] established an
anthropometric measurement guideline for Malnutrition as
wasting or low weight-for-height, which indicates inadequate food intake
causing the child to lose weight; stunting or low
height-for-age, which indicates long-term insufficient nutrient intake
(chronic Malnutrition); and underweight or low weight-for-age
which is a composite index of wasting and stunting. Child
malnutrition is not just about the lack of nutritious food; it is a
combination of multiple causes, such as the frequent occurrence of
disease, poor healthcare practices, accessibility, and other social
services. More than two decades ago, The United Nations International
Children’s Emergency Fund [4] created a conceptual framework that
outlines the multifactorial determinants of child malnutrition. That
includes economic and employment situations, access to food, good
sanitation, awareness, social and institutional practices, program
implementation, and data availability. This framework evolved as it
continuously incorporated new knowledge and evidence on the impacts,
consequences, and causes of Malnutrition.
Several experts identified ancillary factors potentially responsible
for Malnutrition, such as incidence of diarrhoea or acute respiratory
infection (ARI) for the child, food insecurity, low maternal education
and lack of vitamin supplements or fortified food, access to clean
drinking water, sanitation infrastructure facilities, hygiene knowledge
and practices, lack of access to health services, inadequate child
feeding practices and unavailability of food [5]. Food insecurity is a
persistent problem in most countries. According to the 2020 Global
Report on Food Crises (GRCF), as mentioned by [6], ~ 135 million people
in 55 countries and territories were experiencing acute food insecurity
in 2019. Household sanitation reduces the risk of infection and
positively associates with linear growth in children [7].
Adequate nutrition is requisite for human development. Poor nutrition
in the first 1000 days of a child's life can lead to stunted growth,
which is associated with impaired cognitive ability and reduced school
and work performance [8]. Malnourished children fail to attain optimal
growth and development, physical ability to work, and economic
productivity in a later phase of life [1]. Despite the improving
economy and largest anti-malnutrition program, India is among the
countries with the worst child malnutrition level [9]. Malnutrition is
a chronic problem and a longstanding challenge for India. Despite
decades of investment to tackle this problem, India's child
malnutrition rates are still one of the most alarming worldwide, where
the bane of child and maternal Malnutrition is responsible for 15% of
India's total disease [10]. However, malnutrition prevalence is not
equally distributed across India, where vast spatial heterogeneity in
social, cultural, demography, and economy [11]. With these
considerations, a different approach should be adopted to plan policies
and interventions to reduce Malnutrition that will suit a particular
geographical location.
It is evident from the existing literature that there is a need to
examine the spatial distribution of childhood malnutrition in India to
help improve programs by allocating limited resources to priority
districts. Therefore, this study focuses on understanding the spatial
distribution and heterogeneity of Malnutrition across the districts and
states of India and examines the determinants of wasting, stunting, and
underweight in children under the age of five. Spatial analysis using
GIS brings a new approach in understanding priority problems at a broad
scale, thus identifying actual need-based problems and formulating
solutions for the malnutrition crisis in India.
2. Data Source
This study used the secondary data from the National Family Health
Survey (NFHS) of India from 2005-2006 (NFHS-3) and 2015–16 (NFHS-4) at
the state and district level, respectively. The details about the
sampling procedure of the survey can be found in Survey (DHS) under
USAID (https://dhsprogram.com/data/dataset/India_Standard-DHS_2015.cfm?flag=1).
The data factsheets provide comprehensive information on fertility,
mortality, maternal and child health, including child nutrition status
and factors influencing it, such as immediate, intermediate, and
underlying determinants were adopted from the UNICEF conceptual
framework for the states and districts of India. Earlier data of NFHS-3
was limited to state representation covering 29 states with a household
sample size of 109,000 and a sample representing 230,000 women aged
15-49 years and 200,000 below aged five children were tested on health
and nutrition indicators, whereas for NFHS-4 data covered states (29 +
7 union territories) and districts of 640 according to 2011 national
census with a sample size of 566,200 households representing 625,104
women aged 15–49 years and 265,653 below age five children in India).
This study was conducted at the state and the district level covering
two different survey periods, 2005-2006 (NFHS-3) and 2015–16 (NFHS-4).
Comparison between state and district levels is a limitation due to an
unequal number of states and districts from the earlier data set
compared to the latest data of NFHS-4. The digital administrative
shapefile of the state and district of 2005 and 2016 was obtained from
GitHub ( https://github.com/datameet/maps/tree/master/Districts)),
which is shared under Creative Commons Attribution 2.5 India license.
The maps were re-projected in WGS 1984 UTM zone 43N for conducting
spatial analysis. This study did not include parts of Jammu &
Kashmir, as the survey estimates were unavailable for these areas.
2.1 Data Management
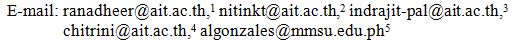
This study classified Malnutrition based on the factors of immediate
determinants, nutrition-specific interventions, and underlying
determinants. The critical determinants of Malnutrition were chosen
based on the conceptual frameworks from previous studies, particularly
UNICEF (1990). Of the many influencing factors from UNICEF Framework,
this study selected specific factors associated with malnutrition
indicators.
- The immediate determinants of child malnutrition are
related to the child's diet and mother's breastfeeding practice,
maternal health condition (e.g. low mother BMI and anemia during
pregnancy), and prevalence of non-communicable diseases (diarrhoea and
acute respiratory infection causing high fever) in a child.
- The nutrition-specific interventions are the programs
by the government [8]. These are classified under maternal healthcare
and supplementation support, such as antenatal care services during
pregnancy and provision of iron and folic acid supplementation in the
first 100 days of pregnancy. Childcare is also another component that
includes immunization and vitamin A supplementation. Government
assistance schemes such as food supplementation to registered
pregnancies in rural areas and financial assistance for institutional
delivery under the JSY program [9].
- The underlying determinants included household
conditions such as sanitation, drinking water sources, access to total
electricity and clean cooking fuel, and early marriage and pregnancy
[11].
3. Method
To analyze the spatial clustering and dependency of child nutrition
outcomes and predictors at the state and district level. A series of
thematic maps were also developed using ArcMap and Geoda using
Geostatistical tools such as Local Indicator Spatial Autocorrelation for
(Univariate Moran's I), and a set of Spatial regression models were
adopted to analyze the factor spatial and child nutrition outcomes.
Finally, the fit model was chosen based on R-Square and AIC (Akaike
information criterion) value. Bivariate LISA is adopted to understand
the spatial relation and dependency between malnutrition indicators and
predictors, illustrated in Figure 2. State and District level thematic
maps were generated to examine the geographical variation of
Malnutrition based on WHO standard classification [12] for assessing the
severity of Malnutrition by percentage prevalence ranges of three
indicators among children less than five years of age were followed.
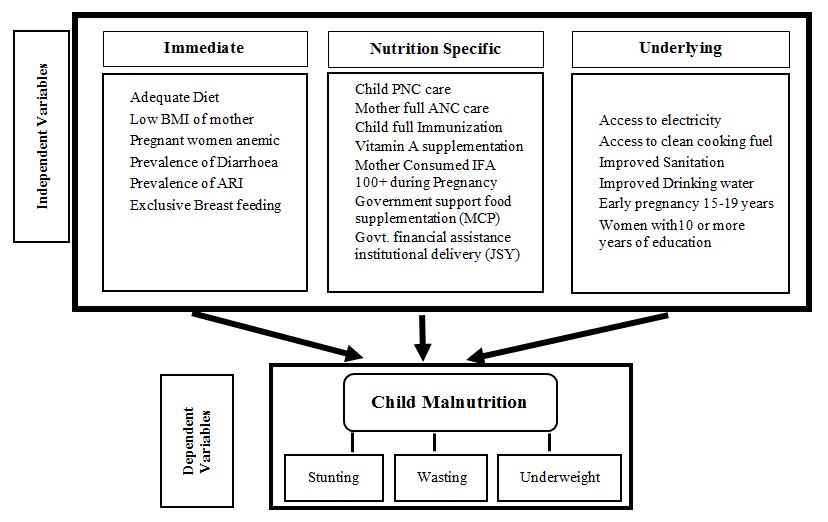
Figure 1: Overall research analysis of relationships of
various variables with dependent variables for child malnutrition
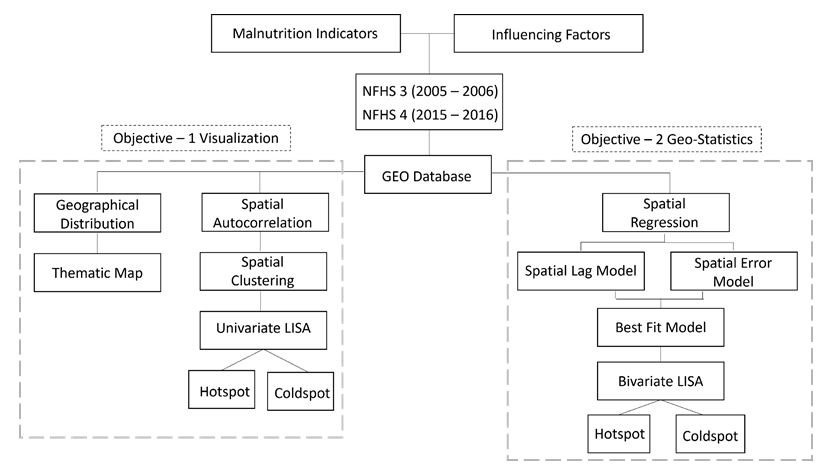
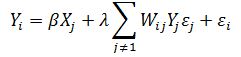
Figure 2: Geospatial data analysis and mapping of
malnutrition in India
To examine spatial clustering of child nutrition outcomes- Spatial
Autocorrelation was performed by Moran's I statistic. The results can
range from -1 to 1, where positive results indicate a positive spatial
correlation while negative results indicate a negative correlation.
Zero result means no spatial autocorrelation or no linear correlation.
The basic formula of Moran's I is as below [15]:
Equation 1
Where:
xi is the value at
ith district,
xj is the value at
jth district,
X̄ is the mean value of the variablex, wij is the weighted coefficient value at (i,j) districts of the weight matrix, and n, m is the spatial units of x.
Local Indicators of Spatial Autocorrelation (LISA) measure the extent
of autocorrelation among the neighbourhood districts. To perform LISA,
a spatial weight matrix was adopted for which a spatial weight matrix
was devised. (w) of first-order using the Queen's contiguity
method (neighbours sharing a common boundary of non-zero length). After
spatial dependency was analyzed, LISA maps are helpful in identifying
the local hotspot and cold spot of a univariate and bivariate variable
over a space. The LISA values allow the computation of its similarity
with its neighbourhood districts and test each location's significance.
In this analysis, five scenarios may take place cluster with high
values - hot spots (districts with high values, with similar
neighbours), cluster with low values – cold spots (districts with low
values, with similar neighbours), and a spatial outlier in which
(districts with high values surrounded by low-value neighbours and
vice-versa) and no significant local autocorrelation [15].
The special choropleth map is a cluster map showing the
locations with a significant local Moran's I statistic
classified by the type of spatial autocorrelation where hotspots are
represented by red colour, blue represents the cold spots, and the light
blue and light red colour is the spatial
outliers. State and District level thematic maps
were generated to examine the geographical variation of Malnutrition
based on WHO standard classification [14] for assessing the severity
of Malnutrition by percentage prevalence ranges of three indicators
among children less than five years of age were followed. To examine
spatial clustering of child nutrition outcomes- Spatial Autocorrelation
was performed by Moran's I statistic. The results can range from -1 to
1, where positive results indicate a positive spatial correlation while
negative results indicate a negative correlation. Zero result means no
spatial autocorrelation or no linear correlation. The basic formula of
Moran's I is as below [15]. The study confirms the significant
spatial autocorrelation in child nutrition outcomes across districts of
India.
Spatial regression models were adopted ("Spatial Lag" and "Spatial
Error" Models) to analyze the spatial influence and relation between
child nutrition indicators and factors influencing. The spatial lag
model assumes that the dependent variable in one area is affected by
the dependent variable nearby. Figure 3 shows the spatial lag model.
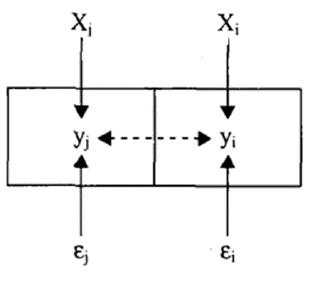
Figure 3: Basic concept for spatial lag model [17]
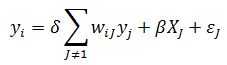
Equation 2
Where:
Yiis a dependent variable denoting the malnutrition
prevalence for the district,
ρ is the spatial autoregressive coefficient,
Wij is a spatial weight matrix and proximity between district
i and j, Yj
is the prevalence of Malnutrition in the district,
β is a vector of regression model coefficients
Xj is the predictor variable, and
εj is a vector of independent and identically distributed error terms [18].
The Spatial Error Model measures the spatial dependency in error terms
and is referred to as nuisance dependence. It assumes that the
residuals correlate in the neighbourhoods of the spatial units (Figure
4).
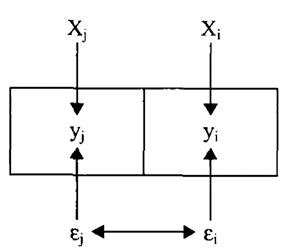
Figure 4: Basic concept for spatial error model [17]
Equation 3
Where:
Yi denotes the prevalence of Malnutrition for the
ith district,
λ is the spatial autoregressive coefficient,
Yj is the prevalence of Malnutrition in the jth district, andW is a spatial weight
matrix used to compute spatial lagged error terms
Wij.
β means regression coefficients of the explanatory
variable and Xj are the predictor variable, and
εiis the residual [18].
4. Results
4.1 Malnutrition Prevalence at State Level
The levels of child malnutrition prevalence map at the state level from
NFHS-3 (2005-06) and NFHS-4 (2015-16) showed all-around improvement
over the last decade. The stunting of children in India was gradually
reduced by 10% in the last few years. However, a striking geographical
disparity was observed where 17 states with an extremely high (>40%)
stunting prevalence in the NFHS-3 survey was reduced to 5 states at
NFHS-4. The states such as Uttar Pradesh, Madhya Pradesh, Jharkhand,
Bihar, and Meghalaya remained with a very high stunting prevalence
which is above the national average of 25% even in NFHS-4. Two states
remained stunted below the national standards of 25% or less stunting
prevalence even after a decade. On the other hand, there was an
improvement in 2 states in 2005-2006 to 14 states in 2015-2016 which
are below the national average.
Wasting, an acute form of Malnutrition, has witnessed an uptick in the
past decade from 2006 to 2016 by 9%. In the last NFHS-4 survey, 28
states suffered from very high wasting (>15%) compared to the
previous 19 states in NFHS-3. With this, child wasting was more
pronounced across India, as shown in Figure 5. According to NFHS-4, out
of 36 states, only Mizoram and Manipur show a low prevalence of child
wasting. States such as Punjab, Andhra Pradesh, Uttar Pradesh, Sikkim,
and Assam are worse in child wasting. The prevalence of children
underweight in India from 2006-2016 remained at a higher scale. Even
after a decade, underweight and an enormous geographical area of India
remained high, as shown in Figure 6. The distribution of Malnutrition
is significantly uneven across the large geographical area of India.
Most states attributing to very high stunting prevalence are clustered
in the country's central (99) and eastern regions (69).
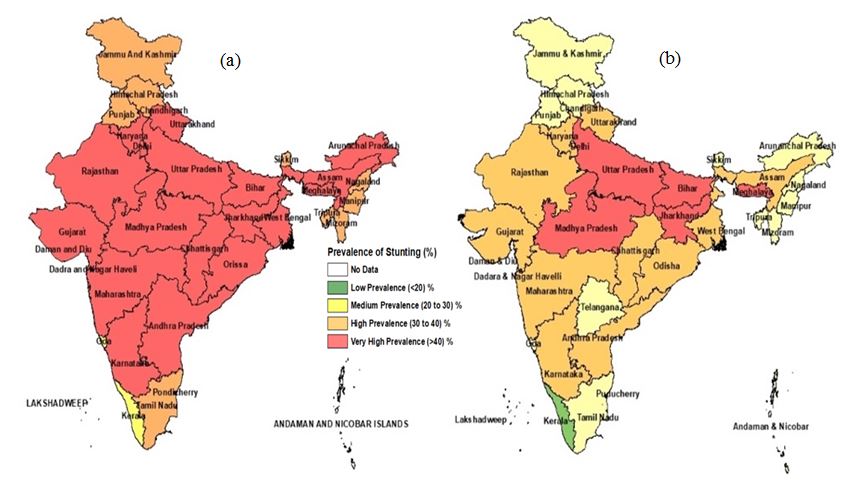
Figure 5: Stunting prevalence of
malnutrition in the last decade (a) 2005-2006 (b) 2015-2016 at the state level in India
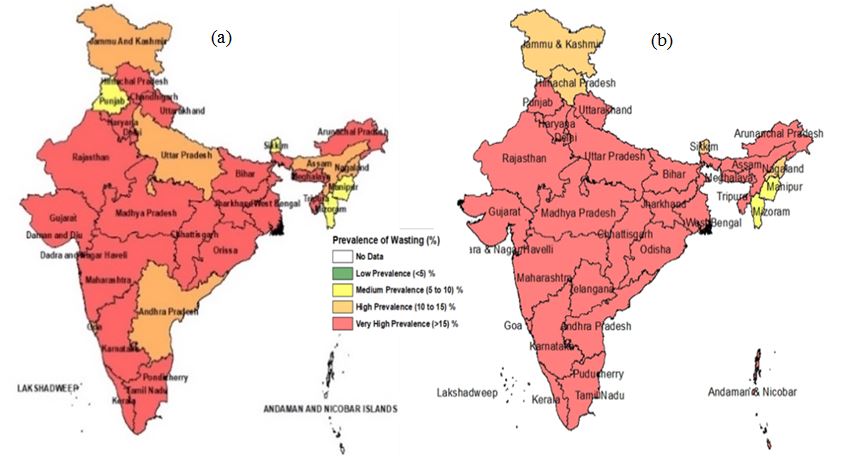
Figure 6: Wasting prevalence of Malnutrition in the
last decade (a) 2005-2006 (b) 2015-2016 at the state level in India
The cluster of very high prevalence is observed in Madhya Pradesh,
Uttar Pradesh, Bihar, and Jharkhand. On the other hand, very high
wasting prevalence is more or less equally occurring in a large
geographic area of India. Districts suffering from a very high waste
are the districts located in the central, east, and south region. This
is particularly the same in the analysis of the state-level stunting
prevalence. Moreover, the underweight prevalence distribution is all
over India and mainly concentrated in the districts of central (139)
and east (91) regions of India.
However, this very high prevalence in states was reduced by 5% from the
NFHS-3 survey to the recent NFHS-4 survey, but medium to high
prevalence doubled over a decade. The situation in Kerala, Northeastern,
and newly formed Telangana states has improved, but Andhra Pradesh's
state has shown degradation to a very high percentage of underweight.
4.2 Malnutrition Prevalence at District Level
District-level malnutrition prevalence in Figure 7 shows high
interstate variation. Child wasting and underweight prevail across a
vast region in India with a clustering distribution. The states that are
not categorized with very high malnutrition prevalence appear to have
districts with very high malnutrition prevalence (Figure 7). Of the 640
districts in India, 237 districts have a very high prevalence of
stunting (>40%), 482 districts with high wasting prevalence
(>15%) and 373 districts are with high underweight prevalence
(>30%). Compared to the developing country's national average for
stunting of 25%, India has 100 districts above the mentioned average,
while 34 districts are above the wasting national average (8.9%). The
established result shows a pattern of concentration and clustering of
districts where Malnutrition is prevalent. The malnutrition indicators
of stunting, wasting, and underweight were noted to consistently occur
in India's central, east, and south zones (Figure 8).
4.3 Spatial Heterogeneity of Malnutrition
The univariate LISA analysis for child malnutrition indicators such as
stunting, wasting, and underweight is represented in Figure 8. The LISA
cluster maps yielded four types of geographical clustering. As
described by [19], the LISA cluster map represents four classifications
of geographical clustering of interest variables. In this study,
"high-high" or hotspots means that areas with above-average
child malnutrition rates also share boundaries with neighbouring
regions with above-average values of the same variables. Whereas
"low-low" or cold spots are the regions with below-average malnutrition
rates that share boundaries with neighbouring regions that have
below-average of the same variable. However, a "high-low" means regions
with below-average values surround the region with above-average
malnutrition indicator rates. Moreover, "low-high" means areas with
above-average values surround below-average malnutrition indicator
values. The three malnutrition indicators show a positive spatial
autocorrelation, among which underweight shows the highest
Moran' I value of 0.712, and 165 districts were found to be hotspots
Figure 9 (On the other hand, the Moran's I value for stunting
was 0.62, which showed 138 districts as hotspots. Wasting,
too, had a positive but low spatial autocorrelation (Moran's I value of
0.461), with 105 districts as hotspot areas.
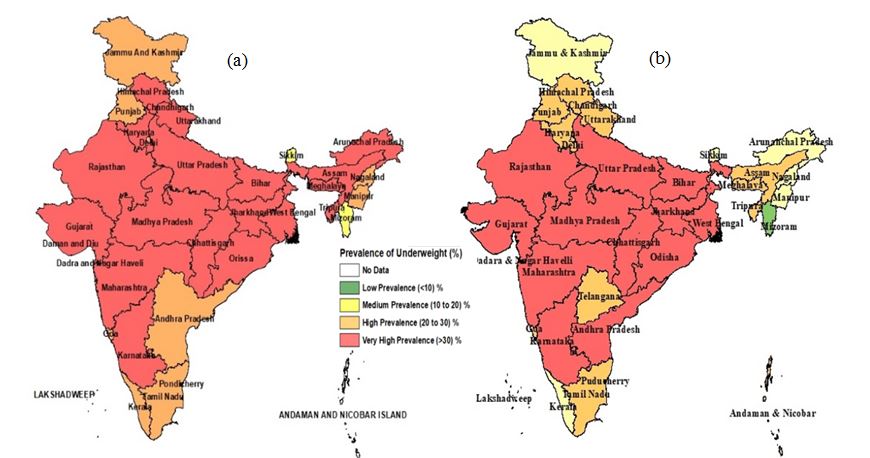
Figure 7: Underweight prevalence of Malnutrition in the
last decade (a) 2005-2006 (b) 2015-2016 at the state level in India
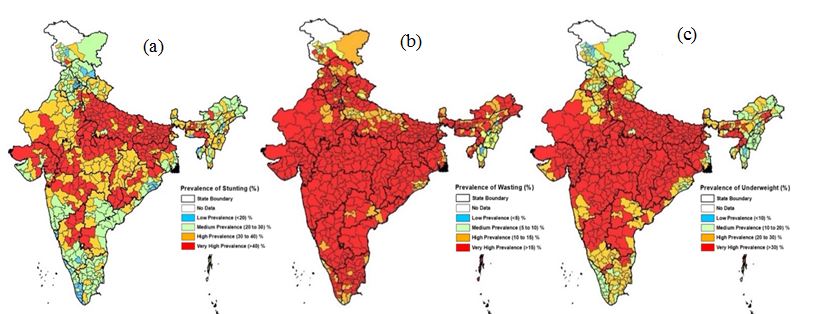
Figure 8: Geographical distribution of
Malnutrition (a) stunting, (b) wasting, and (c) underweight across districts in India
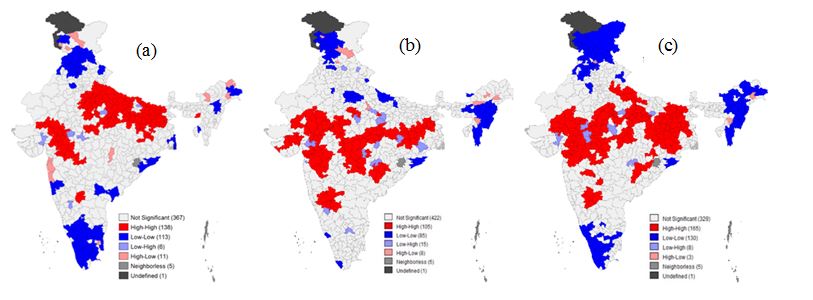
Figure 9: Univariate maps depict spatial clustering and
outliers (a) stunting, (b)wasting, and (c) underweight across districts of India malnutrition
Table 1 presents the relationship between the outcome indicators and
the specific influencing factors. Since there is significant geospatial
clustering in the three outcome variables of Malnutrition, an SEM was
used to understand the spatial relation and strength between child
malnutrition indicators (stunted, wasting, and underweight) and
influencing factors. Furthermore, a spatial correlation analysis was
performed using bivariate LISA to check the geospatial clustering in
the exposure and outcome variable. It is observed that under the
immediate cause, the three forms of Malnutrition (stunting, wasting,
and underweight) are significantly influenced by low mother BMI
(<18.5 kg/m2) and anemia in the mother during pregnancy.
In contrast, the prevalence of diarrhoea and pregnant women having
anemia shows a positive relationship but low influence on the three
malnutrition indicators. On the other hand, children who received an
adequate diet show a significant and negative relation between stunting
and being underweight. Under the nutrient-specific intervention, a
mother receiving complete antenatal care shows a significant negative
relation with stunting and underweight. Whereas both children fully
immunized and receiving vitamin A supplementation shows a low
significant influence with the three malnutrition indicators, while
postnatal care received child shows a low significant influence with
stunting and underweight. Both factors of improved household sanitation
and households using clean cooking fuel are seen to have a negative
relation to child malnutrition. On the other hand, early pregnancy
(15-19 years) shows a positive and significant relation with stunting
and being underweight. The bivariate LISA examined the spatial
relationship between the factors and the outcome variable for the
different geographic areas of India and was used to answer a pertinent
question – is the prevalence of Malnutrition across India constantly
influenced by the identified factors.
Table 1: Spatial Error Model between influencing
factors and outcome indicators
|
Immediate Causes – SEM
|
|
Influencing Factors
|
Stunting Coefficient
|
Wasting Coefficient
|
Underweight Coefficient
|
|
1. Exclusive breastfeeding (6 months)
|
0.102
|
0.033
|
0.123
|
|
2. Adequate diet (6-23 months)
|
-0.18*
|
-0.015
|
-0.209**
|
|
3. Mother with low BMI (<18.5 kg/m2)
|
0.563***
|
0.281***
|
0.702***
|
|
4. Pregnant women anemia
|
0.068***
|
0.051***
|
0.088***
|
|
5. Prevalence of ARI
|
-0.017**
|
-0.030***
|
-0.024***
|
|
6. Prevalence of Diarrhea
|
0.024***
|
0.010
|
0.018**
|
|
Nutrition Specific Intervention - SEM
|
|
1. Mother consumed IFA 100+
pregnancy
|
0.07
|
0.044
|
0.730
|
|
2. Mother had full ANC
|
-0.192***
|
-0.079
|
-0.167***
|
|
3. Child received PNC
|
0.058**
|
-0.001
|
0.057**
|
|
4. The child received Vit A – for 6 months
|
0.095***
|
0.068***
|
0.083***
|
|
5. Child fully immunized
|
0.075***
|
0.055***
|
0.085***
|
|
Underlying Causes - SEM
|
|
1. Households improved sanitation
|
-0.155***
|
-0.070***
|
-0.173***
|
|
2. Households using clean cooking fuel
|
-0.086***
|
-0.044**
|
-0.080***
|
|
3. Households with electricity
|
0.093***
|
0.148***
|
0.136***
|
|
4. Households with improved drinking water
|
0.243***
|
0.068***
|
0.194***
|
|
5. A mother who did not have 10 or more
years of schooling
|
-0.035
|
-0.039
|
-0.039
|
|
6. Early pregnancy (15-19 years)
|
0.22***
|
-0.062
|
0.135*
|
|
***p<0.01, **p<0.05, *p<0.10
|
Table 2: Status of malnutrition indicators using
Bivariate LISA Moran's I values
|
Malnutrition
|
Bivariate
|
Hotspots
|
|
Immediate
|
|
Stunting - Low BMI
|
0.508
|
127
|
|
Wasting - Low BMI
|
0.410
|
113
|
|
Underweight - Low BMI
|
0.642
|
139
|
|
Nutrition Specific Intervention
|
|
Stunting- Antenatal care to Mother
|
-0.458
|
142
|
|
Underweight – Antenatal care for Mother
|
-0.317
|
128
|
|
Underlying Causes
|
|
Stunting – Improved Sanitation
|
-0.508
|
146
|
|
Underweight – Improved Sanitation
|
-0.538
|
147
|
|
Stunting – Early Pregnancy (15-19 years)
|
0.186
|
76
|
Table 2 shows the Bivariate Moran's I statistics for stunting,
wasting, and underweight against the correlates. Results show that the
spatial autocorrelation of underweight, stunting, and wasting with low
mother BMI was 0.64, 0.50, and 0.41, respectively (Table 2). This
indicates a strong association between women's BMI with all three
nutritional indicators.
These findings are consistent with previous studies that mentioned the
influence of women's low BMI would likely have greater malnutrition
prevalence among children [3]. In fact, low mother nutrition is a
significant risk factor for poor fetal development, and undernourished
mothers cannot provide adequate milk during breastfeeding, which
results in Malnutrition in children.
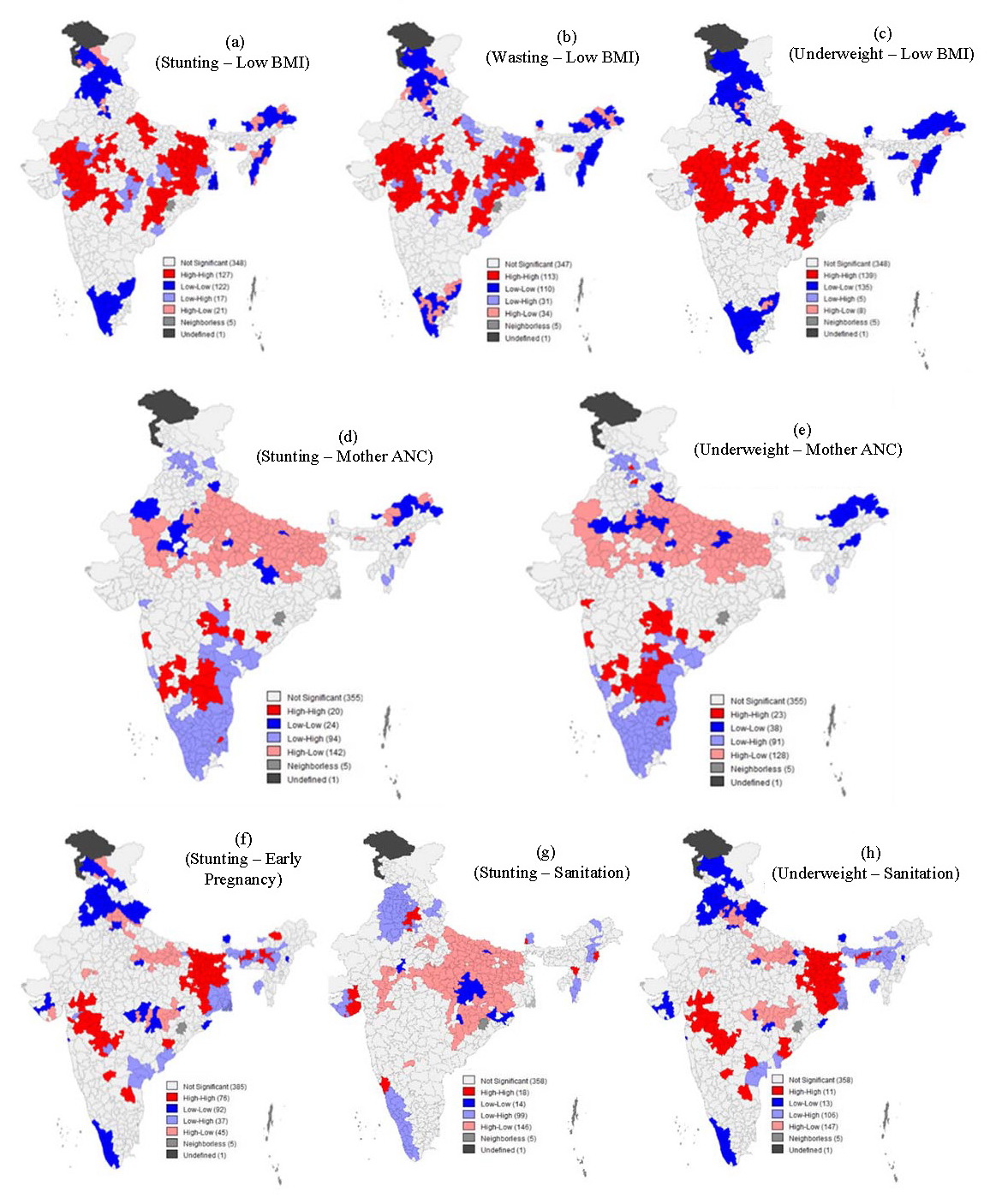
Figure 10: Cluster maps showing the geographic
clustering (hotspots & cold spots) of (a) BMI of mothers vs stunting
(b) BMI of mothers vs underweight (c) mother antenatal care vs stunting
(d) mother antenatal care vs underweight (e) early pregnancy vs
stunting (f) sanitation vs underweight (g) sanitation vs stunting (h)
sanitation vs underweight across districts of India, 2015-16
Generally, the low BMI of the mother showed a high positive spatial
autocorrelation in all three measures of Malnutrition, while antenatal
mother care and improved sanitation are negatively correlated with stunting
and underweight. Moreover, the spatial autocorrelation of stunting and
underweight with improved sanitation was -0.508 and -0.538, respectively
(Table 2).
The bivariate LISA cluster map shows that 127 and 113 districts constitute
hot spots - a high proportion of low mother BMI and a high prevalence of
stunting and wasting, respectively. On the other hand, 122 and 110
districts are observed as cold spots (low proportion of low mother BMI and
low prevalence of stunting and wasting). Similarly, mother antenatal care
showed a negative spatial autocorrelation with stunting and underweight.
Improved sanitation showed high and negative autocorrelation with stunting
and underweight, while early pregnancy indicated a low but positive
relation with stunting. There are 142 out of 640 districts (22%) with the
highest prevalence of stunting in relation to the influencing factor of
antenatal care. Similarly, 20% of the districts in India (128) constitute
the hotspots for underweight antenatal care. These are primarily observed
in Bihar, Uttar Pradesh, and parts of the borders of Madhya Pradesh. In
comparison, the state-level analysis did not capture this point which is
very important for the strategy to improve the situation. Figure 10(a-c)
show the district-level clustering and prevalence of stunting, wasting, and
underweight with a common association with mothers with low BMI (<18.5
kg/m2). Similarly, hotspots for stunting and underweight are
influenced by mother antenatal care, early pregnancy, and sanitation
(Figure 10 (d-e)). The light pink colour on the map represents the
hotspots. Meanwhile, hotspot districts for stunting in relation to early
pregnancy (15-19 years) in Figure 10 f are observed in 78 districts (12%).
Figures 10(g-h) represent the hotspot districts of stunting and underweight
associated with sanitation, indicated in light pink. There are 146 and 147
hotspot districts for stunting and underweight as influenced by low
sanitation. A total of 132 (low-high) hotspot districts are observed where
Uttar Pradesh, Bihar, and parts of the borders of Madhya Pradesh are among
the few. Cold spots (high-low), as represented by the pink colour, occur in
fifty-nine districts and are mainly seen in Kerala, Punjab, Himachal
Pradesh, and a few districts in the northeastern region. At the same time,
403 districts do not have any significant spatial autocorrelation with the
neighbouring districts.
The analysis of prevalence coverage of antenatal care (ANC) to mothers and
underweight (Figure 10(e)) gives a negative spatial autocorrelation, thus,
giving importance to outliers. The light blue colour (low-high) is
considered the hotspot, meaning that districts with mothers not consuming
IFA have high child stunting prevalence. A total of 140 (low-high) hotspot
districts were distributed in central, east, and west regions as well as in
Uttar Pradesh, Bihar, and Madhya Pradesh. The pink colour represents cold
spot areas (high-low) in sixty-seven districts, mainly in Kerala, Punjab,
Himachal Pradesh, and a few districts in the northeastern region. On the
other hand, 335 districts have no significant spatial autocorrelation with
their neighbouring districts. The bivariate LISA result of underweight and
improved sanitation facilities (f) shows a negative spatial autocorrelation
and low Moran's I value (-0.383); thus, outliers are considered more
important. The light blue colour (low-high) is considered the hotspot,
which means that there is a higher prevalence of underweight if there are
poor sanitation facilities. In relation to this, there are 147 (low-high)
hotspot districts distributed in Rajasthan, Madhya Pradesh, Gujarat,
Maharashtra, Chhattisgarh, Odisha, Uttar Pradesh, Bihar, West Bengal,
Karnataka, and Jharkhand. Meanwhile, there are 86 cold spots (high-low)
districts that are indicated in light pink colour which are clustered in the
southern region like Kerala, northeastern region – Nagaland, Mizoram,
Manipur, Assam, and Tripura, in the northern region – Himachal Pradesh,
Punjab, Uttarakhand. On the other hand, stunting and improved sanitation
facilities (g) give a negative spatial autocorrelation, thus, giving
importance to outliers. The light blue colour (low-high) is considered the
hotspot, which means that poor sanitation facilities would result in high
stunting. There are 125 (low-high) hotspot districts that are observed in
Uttar Pradesh, Bihar, and parts of the borders of Madhya Pradesh, Gujarat,
and Maharashtra. The pink colour represents cold spots (high-low). It was
encouraging to find 60 districts in a cold spot which is mainly seen in
Kerala, Punjab, Himachal Pradesh, and a few districts in the northeastern
region.
5. Discussion
Child malnutrition in India continues to be high, and the crisis seems
challenging to solve [1] This study determined the pattern and prevalence
of Malnutrition among children across states and districts of India. Factors
influencing the prevalence of Malnutrition and their geographical
distribution were also examined to determine the high-risk district
clusters. Below are the notable findings from the study.
The analysis results revealed a spatial pattern of stunting, wasting, and
underweight across the states and districts of India. Moreover, based on
the data of NFHS-4, stunting and underweight prevalence across India
witnessed a lower rate of 47% and 28%, respectively, over the last decade,
while wasting prevalence increased by 10%. Of the 640 districts of India,
wasting was highly observed in 75% of the states, followed by underweight
(58%) and stunting (37%). This implies that the most dominant form of
Malnutrition in India is wasting. According to (International Food Policy
Research Institute, 2016), India ranks as the top country in child waste
globally, where 90 per cent of children aged between 6 and 23 months do not
even get the minimum required food.
In addition, a series of spatial clustering maps were developed to find out
the different malnutrition indicators among districts and to determine if
there is a relationship to the malnutrition levels of the neighbouring
districts. Moran's I statistics suggest that there is spatial dependence
and was found highest for underweight (0.71), followed by stunting (0.62)
and wasting (0.46), proving the geographical gradient of Malnutrition in
India. The same observation was obtained by Khan and Mohanty [5] indicating
that malnutrition prevalence among children in India is not distributed
uniformly across districts but instead occurs in clusters. Though there is
a high level of Malnutrition in selected states and regions, a more
significant clustering was observed in the districts of Uttar Pradesh,
Madhya Pradesh, Bihar, and Jharkhand. According to [9], Malnutrition is
scattered across states and the nation as a whole, but it is highly
concentrated among districts in the central regions, particularly in the
rural parts along with the so-called "tribal belt", while the districts in
the southern region are with improved nutritional status. This result can
be linked to the conclusion of [20] that attention needs to be paid to
building neighbourhood health and nutrition profiles and carrying out
interventions based on identified needs.
The spatial analysis suggests a statistically high significant association
of different forms of Malnutrition (stunting, wasting, and underweight)
with the factors such as maternal (status of mother BMI, anemia during
pregnancy, mother antenatal care) and child health (prevalence of Acute
Respiratory Infection (ARI) and diarrhoea, a child receiving Vitamin A and
full immunization) and access to needed household services (improved
sanitation, clean cooking fuel, electricity and improved drinking water).
These factors correlate well with areas where high Malnutrition is
prevailing (central regions), as these are the areas where access to
medical facilities is complicated and limited. The majority of the
mentioned influencing factors on Malnutrition in this study were also proven
by other researchers. According to pieces of literature, poverty, low
women's education, low body-mass-index of mothers, poor sanitation and
drinking water supply, high fertility, increased prevalence of teenage
pregnancies, and lack of immunization are among the influencing factors of
Malnutrition in India [8] and [21]. Studies indicate that there
is a significant relationship between maternal nutritional status with the
well-being of a child [22]. This conclusion supports our findings that the
lack of supplementation of iron and folic acid and non-access to antenatal
care of the mother is the significant influencing factors in child stunting
and being underweight. Failure to supply an adequate amount of nutrients to
meet fetal demand can lead to fetal Malnutrition. The fight against
persistent underweight, stunting, and wasting among children in developing
countries is based on the appropriate maternal nutrition and preventing
micro-nutrient deficiency as their deficiency leads to severe problems
during the gestation period in the mother and stunting in a child after
pregnancy [23].
The spatial relationship between factors and outcome variables indicated
that the hotspots were influenced by the low BMI of the mother, antenatal
care, sanitation, and early pregnancy. These are primarily found in the
districts located in the central regions. This information highlighted the
need for access to the necessities to proceed towards a healthy pregnancy.
At the same time, the child's growth pattern was found to be at lower
levels in most places.
5. Conclusion
This study was based on the notions of the geostatistical pattern analysis
to understand the prevalence of Malnutrition at the state and district
levels in India. The study disclosed that some of the indicators and
contextual factors which cause Malnutrition in an area might be divergent
when viewed at state and district levels. With these results, the
government can focus on addressing other influencing factors on
Malnutrition, such as early pregnancy and antenatal care support.
Therefore, the result of this study would be helpful in further planning
malnutrition interventions as hotspot areas can be identified straight
away. This will eliminate the old practice of implementing a generic
solution to Malnutrition that is often ineffective. Study results suggested
that a district-level strategy should be in place for effective results.
With the influencing factors that have improved along with malnutrition
indicators, the government can strengthen the programs on sanitation, child
immunization, and maternal and childcare support programs. Further, the
annual malnutrition status in India will present a reliable basis for
determining changes in the malnutrition status of children in India. The
study helps the government and NGOs to focus on areas that need attention
to support Malnutrition. Prime Ministers' "Nutrition Mission" initiated in
the year 2017 may also reveal astonishing benefits once the results are
analyzed using the methodology proposed in this study. Malnutrition status
can be better monitored if the government can improve the data collection
process and data analysis using the "mobile app" at village levels and make
them GIS-ready for spatial analysis.
Acknowledgement
This research was conducted for my thesis at the Asian Institute of
Technology under the guidance of a faculty advisor. I am grateful for the
scholarship provided by the Asian Institute of Technology under the Unified
Program with Jawaharlal Nehru Technical University.
References
[1] Global Nutrition Report, (2020). Action on Equity to end
Malnutrition. Bristol, UK, Retrieved from:
https://globalnutritionreport.org/documents/566/2020_Global_Nutrition_Report_2hrssKo.pdf.
[2] Habyarimana, F., Zewotir, T., Ramroop, S. and Ayele, D. G., (2016).
Spatial Distribution of Determinants of Malnutrition of Children under Five
Years in Rwanda: Simultaneous Measurement of Three Anthropometric Indices.
Journal of Human Ecology, Vol. 54(3). 138–149.
https://doi.org/10.1080/09709274.2016.11906996.
[3] World Health Organization, (2010). Nutrition Landscape Information
System (NLIS), Country Profile Indicators Interpretation Guide,
https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1538-4632.1995.tb00338.x.
[4] United Nations International Children’s Emergency Fund,
https://www.un.org/en/academic-impact/unicef.
[5] Khan, J. and Mohanty, S. K., (2018). Spatial Heterogeneity and
Correlates of Child Malnutrition in Districts of India.
BMC Public Health
, Vol. 18(1).
https://doi.org/10.1186/s12889-018-5873-z.
[6] Udmale, P., Pal, I., Szabo, S., Pramanik, M. and Large, A., (2020).
Global Food Security in the Context of COVID-19: A Scenario-Based
Exploratory Analysis. Progress in Disaster Science, Vol. 7.
https://doi.org/10.1016/j.pdisas.2020.100120.
[7] Rah, J. H., Cronin, A. A., Badgaiyan, B., Aguayo, V. M., Coates, S.
and Ahmed, S., (2015). Household Sanitation and Personal Hygiene Practices
Are Associated with Child Stunting in Rural India: A Cross-Sectional
Analysis of Surveys. BMJ Open, Vol. 5(2).
https://doi.org/10.1136/bmjopen-2014-005180.
[8] Singh, S., Srivastava, S. and Upadhyay, A. K., (2019).
Socio-Economic Inequality in Malnutrition among Children in India: An
Analysis of 640 Districts from National Family Health Survey (2015–16).
Int J Equity Health, Vol. 18(1).
https://doi.org/10.1186/s12939-019-1093-0..
[9] Striessnig, E. and Bora, J. K., (2020). Under-Five Child Growth and
Nutrition Status: Spatial Clustering of Indian Districts.
Spat Demogr
, Vol. 8(1), 63–84.
https://doi.org/10.1007/s40980-020-00058-3.
[10] The Global Hunger Index, (2020). One Decade to Zero Hunger Linking
Health and Sustainable Food Systems,
https://www.globalhungerindex.org/pdf/en/2020.pdf.
[11] NITI Aayog Annual Report, (2018–2019).
https://niti.gov.in/sites/default/files/2019-11/AnnualReport2019.pdf.
[12] Menon, P., Nguyen, P. H., Mani, S., Kohli, N., Avula, R. and Tran, L.
M., (2017).
Trends in Nutrition Outcomes, Determinants, and Interventions in India
(2006–2016)
. POSHAN Report 10. New Delhi, India: International Food Policy Research
Institute (IFPRI).
http://ebrary.ifpri.org/cdm/ref/collection/p15738coll2/id/131341.
[13] Food and Nutrition Security Analysis, India, (2019). New Delhi,
India, 2019.
http://ebrary.ifpri.org/cdm/ref/collection/p15738coll2/id/131341.
[14] World Health Organization, (2010). Nutrition Landscape Information
System (NLIS) Country Profile Indicators: Interpretation Guide. 1-38.
https://apps.who.int/iris/handle/10665/44397.
[15] Anselin, L., (1995). Local Indicators of Spatial Association-LISA.
Geogr Anal, Vol. 27(2), 93–115.
https://onlinelibrary.wiley.com/doi/10.1111/j.1538-4632.1995.tb00338.x.
[16] Lee, S., (2001). Developing a Bivariate Spatial Association Measure:
An Integration of Pearson’s r and Moran’s I. J Geogr Syst, Vol.
3(4). 369–385.
https://doi.org/10.1007/s101090100064.
[17] Catma, S., (2021). The Price of Coastal Erosion and Flood Risk: A
Hedonic Pricing Approach. Oceans, Vol. 2. 149–161.
https://doi.org/10.3390/oceans2010009.
[18] Anselin, L., (2002). Under the Hood: Issues in the Specification and
Interpretation of Spatial Regression Models.
Agricultural Economics
, Vol. 27(3). 247–267.
https://doi.org/10.1016/S0169-5150(02)00077-4.
[19] Singh, P., (2011). Performance Pay and Information: Reducing Child
Malnutrition in Urban Slums. Munich Personal RePEc Archive. 1-53.
https://mpra.ub.uni-muenchen.de/29403".
[20] Aijaz, R., (2017). Preventing Hunger and Malnutrition in India.
ORF Issue Brief.
https://www.orfonline.org/wp-content/uploads/2017/06/ORF_IssueBrief_182_Hunger.pdf.
[21] Rao, G., Ladusingh, L. and Pritamjit, R., (2004). Nutritional Status
of Children in North-East India. Asia Pac Popul J, Vol. 19, 39–56.
https://doi.org/10.18356/2d9a4fd8-en.
[22] Narayan, J., John, D. and Ramadas, N., (2019). Malnutrition in India:
Status and Government Initiatives, J Public Health Policy, Vol.
40(1). 126–141.
https://doi.org/10.1057/s41271-018-0149-5.
[23] Black, R. E., Victora, C. G., Walker, S. P., Bhutta, Z. A., Parul
Christian, P., Mercedes de Onis, M., Majid Ezzati, M., Grantham-McGregor,
S., Joanne Katz, J., Martorell, R., Uauy, R. and Maternal and Child
Nutrition Study Group, (2013). Maternal and Child Undernutrition and
Overweight in Low-Income and Middle-Income Countries. The Lancet,
Vol. 382, 427–451.
https://doi.org/10.1016/S0140-6736(13)60937-X.
